Canadian Family Physician
March 1985, Vol. 31, pp. 535-540
H. Kirkaldy-Willis and J. D. Cassidy
Dr. Kirkaldy-Willis is a Professor Emeritus of Orthopedics and director of the Low-Back Pain Clinic at the University Hospital, Saskatoon, Canada.
FROM ABSTRACT:
Spinal manipulation, one of the oldest forms of therapy for back pain, has mostly been practiced outside of the medical profession.
Over the past decade, there has been an escalation of clinical and basic science research on manipulative therapy, which has shown that there is a scientific basis for the treatment of back pain by manipulation.
Most family practitioners have neither the time nor inclination to master the art of manipulation and will wish to refer their patients to a skilled practitioner of this therapy.
Results of spinal manipulation in 283 patients with low back pain are presented.
The physician who makes use of this resource will provide relief for many patients.
THESE AUTHORS ALSO NOTE:
About 80% of the population will experience low back pain sometime during their adult life.
At any given time, 20-30% of the adult population is suffering from low back pain.
Low back pain is second only to upper respiratory infections as the cause of worker loss of productivity.
“Most causes of low back pain lack objective clinical signs and overt pathological changes.”
“Less than 10% of low back pain is due to herniation of the intervertebral disc or entrapment of spinal nerves by degenerative disc disease.”
“Spinal manipulation is essentially an assisted passive motion applied to the spinal apophyseal and sacroiliac joints.”
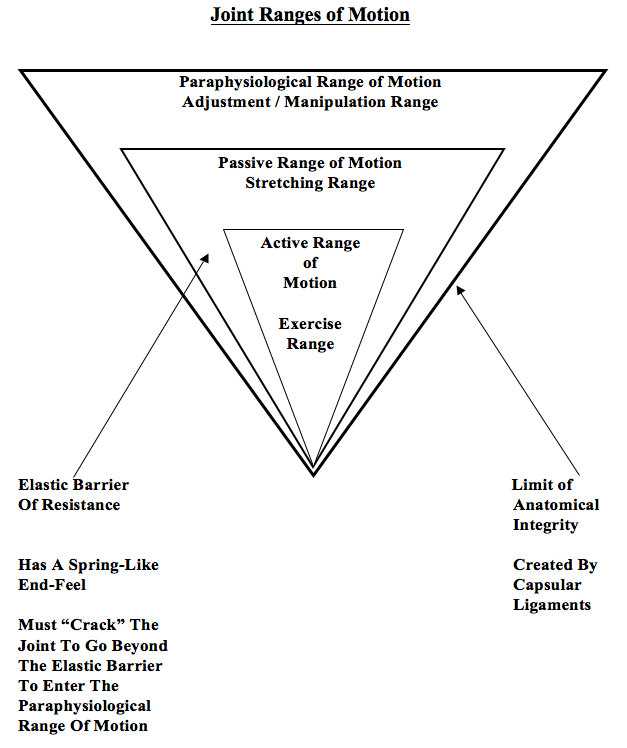
There are three categories of joint motion:
1) Active range of motion.
2) “Beyond the end of the active range of motion of any synovial joint, there is a small buffer zone of passive mobility.” A joint can only move into this zone with passive assistance, and going into this passive range of motion “constitutes mobilization.” [This is mobilization, not manipulation.]
3) “At the end of the passive range of motion, an elastic barrier of resistance is encountered. This barrier has a spring-like end-feel.”
“If the separation of the articular surfaces is forced beyond this elastic barrier, the joint surfaces suddenly move apart with a cracking noise.”
“This additional separation can only be achieved after cracking the joint and has been labeled the paraphysiological range of motion.”
“This constitutes manipulation.” [Important]
“The cracking sound on entering the paraphysiological range of motion is the result of sudden liberation of synovial gases—a phenomenon known to physicists as cavitation.”
Following cavitation, a synovial bubble can be observed on x-rays, which is reabsorbed over the following 30 minutes. During this “refractory period” there is no resistance between the passive and paraphysiological zones.
“At the end of the paraphysiological range of motion, the limit of anatomical integrity is encountered. Movement beyond this limit results in damage to the capsular ligaments.”
Joint manipulation [adjusting] “requires precise positioning of the joint at the end of the passive range of motion and the proper degree of force to overcome joint coaptation” [to overcome the resistance of the joint surfaces in contact].
“With experience, the manipulator can be very specific in selecting the spinal level to be manipulated.”
Melzack and Wall proposed the Gate Theory of Pain in 1965, and this theory has “withstood rigorous scientific scrutiny.”
“The central transmission of pain can be blocked by increased proprioceptive input.” Pain is facilitated by “lack of proprioceptive input.” This is why it is important for “early mobilization to control pain after musculoskeletal injury.” [Important]
The facet capsules are densely populated with mechanoreceptors. “Increased proprioceptive input in the form of spinal mobility tends to decrease the central transmission of pain from adjacent spinal structures by closing the gate. Any therapy which induces motion into articular structures will help inhibit pain transmission by this means.” [Important]
Stretching of facet joint capsules will fire capsular mechanoreceptors which will reflexly “inhibit facilitated motoneuron pools” which are responsible for the muscle spasms that commonly accompany low back pain.
In chronic cases, there is a shortening of periarticular connective tissues and intra-articular adhesions may form; manipulations [adjustments] can stretch or break these adhesions.
“In most cases of chronic low back pain, there is an initial increase in symptoms after the first few manipulations [probably as a result of breaking adhesions]. In almost all cases, however, this increase in pain is temporary and can be easily controlled by local application of ice.” [Important]
“However, the gain in mobility must be maintained during this period to prevent further adhesion formation.” [Important]
“At present, there is no evidence that manipulation replaces subluxated vertebrae. This theory was first put forward by the chiropractic profession many years ago and has largely been abandoned.” [Many, including myself, largely disagree with this statement.]
These authors do not recommend manipulation in cases of prolapsed disc with “marked neurological deficit.”
These authors present the results of a prospective observational study of spinal manipulation in 283 patients with chronic low back and leg pain. All 283 patients in this study had failed prior conservative and/or operative treatment, and they were all totally disabled (“Constant severe pain; disability unaffected by treatment.”)
These patients were given a “two or three week regimen of daily spinal manipulations by an experienced chiropractor.”
“No patients were made worse by the manipulation, yet many experienced an increase in pain during the first week of treatment. Patients undergoing manipulative treatment must therefore be reassured that the initial discomfort is only temporary.”
“In our experience, anything less than two weeks of daily manipulation is inadequate for chronic low back pain patients.” [Very Important]
These authors considered a good result from manipulation to be:
1) “Symptom-free with no restrictions for work or other activities.”
2) “Mild intermittent pain with no restrictions for work or other activities.”
81% of the patients with referred pain syndromes subsequent to joint dysfunctions achieved the “good” result.
48% of the patients with nerve compression syndromes, primarily subsequent to disc lesions and/or central canal spinal stenosis, achieved the “good” result.
Radiographic evidence of motion segmental instability (from maximum flexion–extension lateral views) “was associated with a significantly poorer response to manipulation.”
“The physician who makes use of this [manipulation] resource will provide relief for many back pain patients.”
KEY POINTS FROM THIS ARTICLE
1) 80% of the population will experience low back pain during their adult life.
2) At any given time, 20-30% of the adult population is suffering from low back pain.
3) “Less than 10% of low back pain is due to herniation of the intervertebral disc or entrapment of spinal nerves by degenerative disc disease.”
4) Moving of a joint beyond the passive range of motion, past the elastic barrier, and into the paraphysiological space, requires “cracking” of the joint; this is their definition of manipulation [adjustment].
5) “Cracking” of the joint causes the patient no harm or damage.
6) “At the end of the paraphysiological range of motion, the limit of anatomical integrity is encountered. Movement beyond this limit results in damage to the capsular ligaments.”
7) These authors propose that manipulation inhibits pain by firing facet capsule mechanoreceptors, which in turn close the pain gate for the central transmission of pain.
8) In chronic low back pain, there is shortening of periarticular connective tissues and intra-articular adhesions may form. Manipulations [adjustments] can stretch or break these adhesions, which may give the patient a temporary increase in symptoms. This increase in symptoms should be controlled by the application of ice, not by abandoning additional manipulations [adjustments]. If manipulations [adjustments] are stopped, “further adhesion formation” may occur.
9) These authors do not recommend manipulation in cases of prolapsed disc with “marked neurological deficit.”
10) These authors show that specific chiropractic adjustments can essentially “fix” 81% of referred joint dysfunction and 48% of nerve compressive back pain syndromes in patients that are completely disabled and who have failed all prior treatment (including surgery), if they are appropriately adjusted daily for a period of at least 2 – 3 weeks.
11) “No patients were made worse by the manipulation, yet many experienced a increase in pain during the first week of treatment. Patients undergoing manipulative treatment must therefore be reassured that the initial discomfort is only temporary.”
12) “In our experience, anything less than two weeks of daily manipulation is inadequate for chronic low back pain patients.” [Very Important]
13) Radiographic evidence of motion segmental instability (from maximum flexion–extension lateral views) “was associated with a significantly poorer response to manipulation.”
14) “The physician who makes use of this [manipulation] resource will provide relief for many back pain patients.”