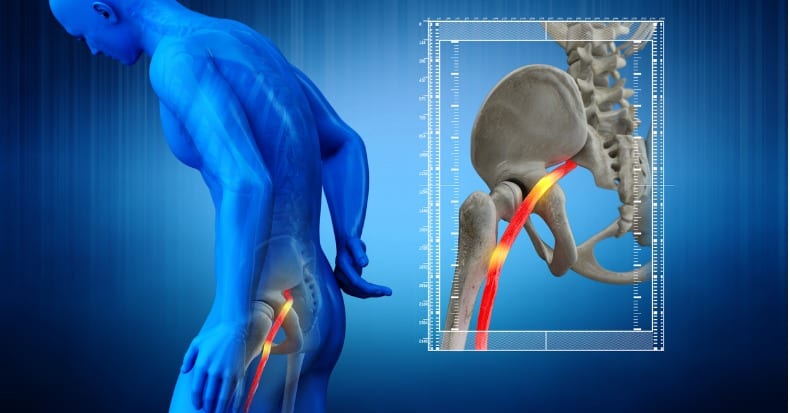
The roots of the sciatic nerve exit the spine through several levels in the lower back, join in the buttock region, and travel down into the lower extremities. When pressure is applied to the sciatic nerve in the lower back area, it can generate pain and other sensations down the nerve into one of the legs—a condition we commonly refer to as sciatica.
In younger and middle-aged adults, the most common cause of sciatica is a herniated disk in the lower back in one or more locations. Because of the structure of the sciatic nerve, the characteristics of the patient’s symptoms can direct their doctor of chiropractic on where to look for potential causes in the lower back:
- S1-2 Level (S1 nerve root): outer foot numb, difficulty walking on toes, weak Achilles tendon reflex
- L5-S1 Disk (L5 nerve root): inner foot numb, weak big toe and heel walking, no reflex changes
- L4-5 Disk (L4 nerve root): shin numb, weak heel walking, patellar tendon reflex loss
- L3-4 Disk (L3 nerve root): medial knee numb, weak walking up steps, weak patellar tendon reflex
- L2-3 Disk (L2 nerve root): front of thigh pain/numb, weak walking up steps, positive patellar reflex
- L1-2 Disk (L1 nerve root): groin pain/numb, weak squat and steps, no deep tendon reflex
- T12-L1 Disk (T12 nerve root): buttock numb, weak lower abdominal muscles, possible spinal cord compression
In sciatica patients under 55 years of age, the two lowest disks in the lower back—the L4-5 and L5-S1—are the culprit 95% of the time. The good news is that a systemic review of 49 published studies found that spinal manipulative therapy, the primary form of care provided by doctors of chiropractic, is an effective non-surgical treatment option for relieve local and radiating pain in patients with a herniated disk in the lower back.
Even though sciatic pain is often initially sharp and severe, most cases can by successfully managed non-surgically within three to six weeks; however, a referral to a specialist or a referral for advanced imaging (such as an MRI) may be necessary to identify additional pain sources if the patient’s pain persists. Surgery is usually restricted to those who have neurological loss and/or bowel or bladder control problems (the latter may become emergent in order to avoid permanency). As with many musculoskeletal conditions, the sooner one seeks care in the course of the disease, the more likely (and the faster) they will achieve a successful treatment outcome.